Integrating Planetary Health into the Medical Curriculum
Development Education and Health
Abstract: Planetary health is a field that looks at human-caused disruptions to the environment and the effect that these disruptions have on human health. We are living in a world where experts have declared a ‘code red’ for both the planet and human health – hence, planetary health is an area of increasing and urgent importance. Health professionals of all levels need to be aware of the relationship between climate change and health. Education on this should begin at the medical student level, ideally building on first and second level education for all. Medical students around the world have been calling for teaching in this area, and in many cases are leading the movement. Globally, there is a shift amongst third level educators to provide education on planetary health. In their 2018 Outcomes for Graduates, the General Medical Council in the United Kingdom (UK) introduced a new learning outcome on sustainable healthcare, which has served as leverage for educators in the UK to implement new planetary health teaching.
Current teaching on planetary health at the university level in Ireland is inconsistent and inadequate. There are no defined learning outcomes for medical students in Ireland as seen in the UK. In the absence of same, groups such as Irish Doctors for the Environment and the Climate and Health in Medical Education (CHIME) network have been making efforts to develop a framework for planetary health teaching which could be implemented at both a national and international level. This article will discuss the work of these groups so far. It will outline how we can overcome some of the barriers and facilitators to integration, and will also provide examples of learning outcomes that can be incorporated easily into current curricula without requiring significant change. A changing climate requires a changing curriculum, and educators must build on the global momentum with the urgency that this crisis requires.
Key words: Planetary health; Medical education; Climate change; Sustainable healthcare.
Introduction
Planetary health is an interdisciplinary field that examines human-caused disruptions to the environment and the effect that these disruptions subsequently have on human health. The concept was launched in 2015 by the Rockefeller Foundation-Lancet Commission, which defined the term as ‘The health of human civilization and the state of the natural systems on which it depends’ (Whitmee et al., 2015: 1978).
Over the past 60 years, humans have been exerting pressure on the planet at unprecedented rates. The global population has increased from an estimated 3 billion in 1960 to 7.8 billion in 2021 (United Nations Population Fund, 2022), and is projected to reach 9.7 billion by 2050 (United Nations, 2022). Energy use went from 100 exajoules in 1960 to over 450 exajoules in 2010 (Vlachogianni and Valavanidis, 2013), with corresponding jumps in water use, fertiliser consumption, transport use, paper and plastic production (Myers, 2017). This has in turn led to degradation of the biosphere, through drastic rises in ocean acidification, tropical forest loss, marine fish capture and carbon dioxide use (Ibid). In 2019, the Intergovernmental Science Policy-Platform on Biodiversity and Ecosystem Services (IPBES) - a United Nations-based organisation which provides an interface between science and policy on biodiversity - released a report estimating that one million species of plants and animals are at threat of extinction (IPBES, 2019).
Health experts have become increasingly aware of the health impacts of the climate and biodiversity crises. Environmental issues such as air pollution, food and water insecurity, expanding ranges of infectious disease vectors, extremes of temperatures and natural disasters are urgent and pressing threats to human health worldwide. Indeed, the World Health Organisation has declared climate change to be the ‘single biggest health threat facing humanity’ (World Health Organisation, 2022). Tackling climate change and biodiversity loss is also essential to the achievement of the United Nations (UN) Sustainable Development Goals (SDGs) and the recognition of human rights globally. It is well-recognised that climate change disproportionately affects those who are least responsible and most vulnerable: the global South, indigenous communities, and women and girls. Thus, while climate change is directly related to a number of the SDGs (for example Goals 6, 7, 11 and 13), it implicitly affects every SDG (UN Department of Economic and Social Affairs, 2022). Global temperature rise is currently at 1.2 degrees above pre-industrial levels, and experts from the Intergovernmental Panel on Climate Change (IPCC) have warned that we must stay below 1.5 degrees by the end of this century in order to avoid irreversible damage to our planet and societies (IPCC, 2018). Based on the latest targets and negotiations from the 2021 UN Conference of Parties (COP) 26 meeting in Glasgow, an international climate research group has estimated that we are currently on a path of a highly dangerous 2.4 degrees of warming (Climate Action Tracker, 2021).
In their 2021 report, the IPCC states: ‘It is unequivocal that human influence has warmed the atmosphere, ocean and land’, adding that ‘widespread and rapid changes in the atmosphere, ocean, cryosphere and biosphere have occurred’ (IPCC, 2021: 5). It concludes that only rapid and drastic cuts in greenhouse gas emissions will allow us to prevent disastrous global warming. The UN Secretary-General, Antonio Guterres, declared the report a ‘code red for humanity’ (United Nations, 2022). In September 2021, a joint editorial published by over 200 health journals worldwide reinforces this sentiment, and warns of ‘catastrophic harm to health that will be impossible to reverse’ (Atwoli et al., 2021: e1). The Lancet Countdown on Health and Climate Change, an international collaboration that monitors the evolving health profile of climate change, echoes the IPCC by declaring a ‘code red for health’ in their 2021 report (Romanello et al., 2021).
Relevance of planetary health to the medical curriculum
If the world’s leading medical journals are publishing highly cited editorials highlighting the enormous threat that the climate crisis poses to human health, and urging that health professionals take immediate action, then it begs the question: what is being done to prepare doctors for this unprecedented challenge? Universities are the places where the scientists, doctors, thinkers and leaders of the future are educated, and are thus the institutions in which this action must begin. Climate change education and advocacy must become a core part of their function. While this applies to all streams of healthcare professional students, the focus in this article will be on the medical curriculum.
Climate change acts as a force multiplier, interacting with, and exacerbating many existing determinants of health and disease such as poverty, migration and air quality. It, therefore, has the potential to affect almost every aspect of health and, therefore, every field of medicine. Indeed, increased morbidity and mortality attributable to climate change is already being documented in Europe and across the world due to cardiovascular, respiratory and infectious disease, injury and mental health effects amongst others (Romanello et al., 2021). Effectively preparing medical students for a career in treating patients, necessitates a comprehensive understanding of the intricate relationship between the health of a person and their environment. This necessity is reflected in new guidance from leading medical regulatory bodies such as the UK’s General Medical Council, who have updated their Outcomes for Graduates to include the following: ‘Newly qualified doctors must be able to apply the principles, methods and knowledge of population health and the improvement of health and sustainable healthcare to medical practice’ (General Medical Council, 2018: 23).
Including climate change (within the wider planetary health and sustainability contexts) in the medical curriculum will foster climate change preparedness, promote public health and eco-health literacy, and better prepare graduates for the challenges they will face (Maxwell and Blashki, 2016). Furthermore, climate change and health equity are inextricably linked; as a risk amplifier, climate change worsens existing health vulnerabilities and inequalities (Haines and Patz, 2004). Thus, as outlined above, addressing climate change is a prerequisite for meeting many of the SDGs, particularly Goal 1 (no poverty), Goal 2 (no hunger) Goal 3 (good health and well-being) and Goal 10 (reduced inequalities), with many other SDGs also directly implicated.
Finally, the healthcare sector itself contributes to a significant proportion of global greenhouse gas emissions. If the healthcare sector were a country, it would be the world’s fifth largest emitter (Carbon Brief, 2022). There is an urgent need to decarbonise the world’s healthcare systems in order to meet the targets agreed in the Paris Agreement, and healthcare workers will have to play a leading role in this action. Recognising this need, the UK’s National Health Service (NHS) became the world’s first healthcare service to declare their intention of rapidly achieving net zero emissions, stating:
“Our intention is to construct the most ambitious, credible declaration to reach net zero of any national healthcare system in the world. However, they can only be delivered if they are supported by collective action from all NHS staff” (National Health Service, 2020: 14).
The role of the physician in planetary health action
There is already a large literature base making a case for the inclusion of planetary health and sustainable healthcare in medical teaching. The role of the physician as an interface between the public and the realm of science is mentioned in the literature as a potential means for increasing planetary health awareness within society at-large (Gómez et al., 2013). Harnessing the potential of this leadership role to have a positive influence in society with respect to planetary health issues requires the proper education of medical students on these topics (Walpole et al., 2016).
The potential that climate change and environmental instability have to act as a catalyst in redefining the role of the physician as a socially-conscious and eco-literate advocate for global health begins with undergraduate medical training (Maxwell and Blashki, 2016; McKimm and McLean, 2011; McLean, Gibbs and McKimm, 2020). As Huss et al. (2020: 1098) outlines, integrating ‘sustainable healthcare’ into curricula should seek to promote ‘a deep understanding of global issues including environmental sustainability and universal values such as justice, respect for all humanity and equality’ and would develop critical thinking skills, social empathy and self-awareness amongst students, qualities that are crucial to any development education.
Medical student calls for planetary health teaching
This growing literature base is accompanied and indeed augmented by increased medical student demand for planetary health teaching. Since the launch of the ‘planetary health’ concept in 2015, medical students have been calling for its inclusion into the medical curriculum. In 2018, the International Federation of Medical Students’ Associations (IFMSA), which represents over 1.3 million medical students globally, released a statement calling for the integration of climate change into healthcare curricula worldwide (IFMSA, 2018).
The literature further underlines the student-perceived lack of planetary health teaching in medical education. Liao et al. (2019) found that 80 per cent of medical students surveyed in China admit inadequate knowledge on climate change and health. In an often-cited survey, 34-40 per cent of United States (US) graduates in 2009-2013 believe their instruction on environmental health was inadequate (Finkel, 2019). Omrani et al. (2020) found that of 2,817 schools in 112 countries surveyed, only 15 per cent report formal teaching on the health effects of climate change on health. An additional 12 per cent of schools have informal teaching through student-led activities, demonstrating the student enthusiasm for planetary health teaching even outside of the formal curriculum. Shah and Owusu-Addo (2021) note that for final year students, time-constraints and content-overload are potential barriers to curriculum change; they suggest that problem-based learning could be a potential route for planetary health integration with the pre-existing curriculum.
Hampshire et al. (2021) assess student perceptions on inclusion of planetary health teaching at twelve US medical schools. Of 600 respondents, 84 per cent believe that climate change and its health effects should be part of the core medical curriculum. At Yale University, 63 per cent of surveyed medical, nursing and physician assistant students agree that the links between climate change and health should be covered in the classroom and reinforced in the clinical setting (Ryan, Dubrow and Sherman, 2020). In China, the majority of the surveyed medical students agree that the health impacts of climate change should be included in their current curriculum (Liao et al., 2019). Similar studies of the perceptions of European medical students could not be located in the literature, suggesting a need to increase research in this area to guide planetary health curriculum development in Europe.
Medical students have a unique role as a catalyser for curriculum change, being ideally positioned to advocate training on climate change and medicine (Rabin, Laney and Philipsborn, 2020). Student-led initiatives are driving the inclusion of planetary health into medical education worldwide. Students at Emory University in the US, in cooperation with motivated faculty, have created a disseminated climate change pre-clinical curriculum which is planned to be incorporated into the curriculum for the class of 2024 (Ibid). In the UK, medical students participated in the extensive consultations that eventually led to the previously described outcome on sustainable healthcare (General Medical Council, 2018). The Health and Environment Adaptive Task force (HEART), a subgroup within the Canadian Federation of Medical Students (CFMS), has created a set of core curricular competencies to drive curricular change in Canadian medical schools (CFMS, 2019).
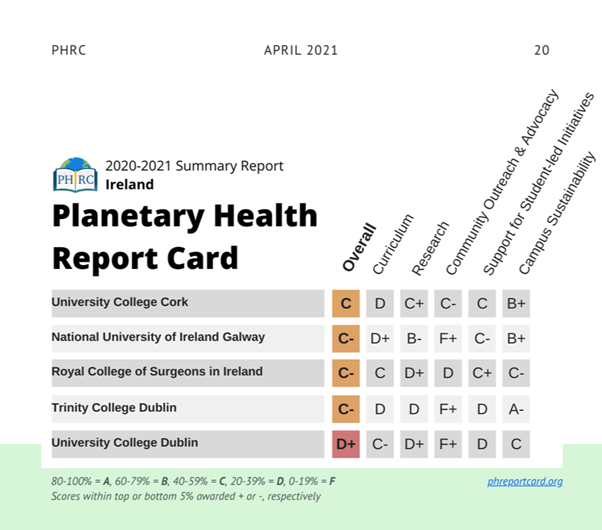
The Planetary Health Report Card (PHRC, 2021) is another such example. The PHRC is a student-led initiative to evaluate planetary health engagement in medical schools. Founded in 2019 by medical students at University California San Francisco, the initiative has expanded internationally to include schools across the US, Canada, the UK, Ireland and Germany. The PHRC provides standardised metrics designed by students and faculty experts that medical students worldwide can use to review and compare their home institutions. The metrics grade medical schools in five discrete categories: curriculum, research, support for student-med initiatives, community outreach and advocacy, and campus sustainability. The resulting report card displays the grades A to F achieved in each category and overall, providing an effective means of communicating the outcomes to school administration and students, as well as the public.
Teaching methods and content
In response to these calls from health professionals, educators and students, how do we best go about integrating planetary health into medical curricula? One of the key pieces of existing research identified was performed by Tun (2019); researchers carried out semi-structured interviews with a diverse range of medical educators in order to establish barriers and facilitators towards the integration of sustainable healthcare in medical education. The main barriers and facilitators that emerged from this study are summarised in Table 1.
Table 1. ‘Barriers and facilitators’ from Tun (2019).
| Barriers | Facilitators |
|
1. Lack of knowledgeable teacher 2. Lack of space 3. Uncertainty of location 4. Need for learning resources 5. Difficulty in assessment 6. Emotional impact needing resistance |
1. Competition between institutions 2. Demand from students 3. Shift towards sustainability in higher education 4. GMC mandate 5. Leadership in other stakeholders 6. Support and resources |
In a previous study by Walpole and Mortimer (2017), seven medical schools participated in a nine-month collaborative project in which they endeavoured to develop, deliver and evaluate a teaching programme on sustainable healthcare. The authors highlight three salient findings:
1. A collaborative approach that allowed discourse between levels of expertise, experience and different institutions conveyed significant benefit in achieving the project’s aim.
2. Topics of sustainability are suitable for teaching across a broad range of pedagogies and do not detract from the development of ‘generic skills and other core knowledge’.
3. Curriculum development should be based on ‘established and coherent’ learning outcomes.
In order to facilitate ease of implementation, some authors recommend that planetary health teaching be incorporated into already existing content or that existing material be broadened to accommodate planetary health themes (Bell, 2010; Iroku-Malize, Keber and Phillipe, 2017; Walpole and Mortimer, 2017). Use of didactic learning and case-based teaching in tandem is suggested; with the didactic teaching as a means of presenting the topics to the students in a broad sense and the case-based learning as a method of highlighting the effects of these issues through a more specific, individual lens (Hackett et al., 2020; Walpole and Mortimer, 2017). Taking advantage of modern technology and utilising e-learning is also a method advocated in the literature (Musaeus et al., 2018). Furthermore, Green and Legard (2020) make recommendations for peer learning through the medium of e-technologies as the optimum means of delivering planetary health teaching. In terms of the location of content, the most prominent argument made is for the spiralling of planetary health content throughout curriculum, in that topics would be introduced in the first year of study and then built upon in subsequent years (Teherani et al., 2017; Collins et al., 2018) .
In 2014, Walpole et al. (2015) conducted a UK-wide consultation using a Delphi-process to garner opinions of healthcare students, healthcare educators and other key stakeholders in order to draft learning outcomes for the delivery of environmental sustainability teaching in medical education. The first learning outcome, ‘describe the relationship between the natural environment and human health’, assesses student-knowledge on environment-mediated health-effects through the lens of planetary health. The second; ‘discuss the duty of a doctor to protect health in a time of global environmental change’ relates to environmental stewardship and the acknowledgement of the responsibility of the physician to regard health holistically, with an awareness of the determinants of health. The third; ‘demonstrate skills for a sustainable health system’ relates to utilising information about planetary health to assess and improve decisions about health services delivery. These domains have since been refined (Thompson et al., 2014) and piloted (Walpole et al. 2016, 2017, 2019) in medical education.
A growing planetary health movement
Internationally, there are numerous institutions that promote and campaign for the integration of planetary health in healthcare education. The Centre for Sustainable Health Care (CSH, 2022) in the UK provides education and training on sustainable healthcare through fellowships, online courses and support for quality improvement projects. The Planetary Health Alliance based in the US (PHA, 2022) shares educational resources and provides a network for planetary health educators to connect. The European NurSuS Toolkit project was developed to provide teaching in sustainability for nurses (NurSuS, 2022).
However, despite the evidence and the supports available, medical schools have been slow to encorporate planetary health teaching into their curriculum. The second annual PHRC, published in April 2021, assessed 62 medical schools across the US, Canada, UK, Ireland and Malaysia (PHRC, 2021). The results show inadequate education and engagement in planetary health and sustainable healthcare by medical schools globally, particularly in the domain of curriculum content.
The Irish setting
Planetary Health Report Card in Ireland
Irish medical schools were included in the PHRC for the first time in the 2020/2021 academic year by student members of Irish Doctors for the Environment (IDE). Student members from five of the six Irish medical schools were responsible for evaluating their own institution. Faculty at each school were alerted to the process and asked for assistance in cases where students were unable to find information on their own. Information was sought from available information online, by contacting relevant staff, speaking to senior students, and by requesting access to curriculum overviews and programme learning outcomes from the school administrations.
The grades achieved by Irish medical universities range from a C in University College Cork (UCC) to a D+ in University College Dublin (UCD) (PHRC, 2021). Results are shown in Figure 1. Very few learning outcomes in Irish medical curricula directly address or include the concept of planetary health or climate change, and inclusion of specific topics seems to remain reliant on individual lecturers’ interest. While most universities are found to have excellent research institutes covering specific aspects of planetary health, the links between these institutes and medical schools have not been created. This is an important area for development and improvement, as interdisciplinary collaboration is key to ensuring effective education in this field.
Figure 1. ‘PHRC Findings for Irish universities’ in PHRC (2021)
In a report on the findings, currently in press, the students provide recommendations to improve planetary health teaching in Ireland. The recommendations, addressed to the medical schools and the Irish Medical Council, will include the following:
1. Develop a national standard on planetary health education;
2. Encourage schools to collaborate and use pre-existing planetary health resources;
3. Integrate planetary health to all parts of the curriculum;
4. Join international calls and networks on planetary health.
Climate and Health in Medical Education (CHIME) Ireland
In response to the growing importance of planetary health teaching and in the absence of any described syllabus in the Irish setting, health professionals and third-level educators in Ireland came together in 2020 to form Climate and Health in Medical Education (CHIME) Ireland. The group is composed of representatives from seven universities representing all medical schools across the island of Ireland. The project has brought students together with academic staff to discuss what should be included in a planetary health curriculum for medical students.
CHIME has a number of objectives:
1. To form a network of population health educators from all Irish medical schools;
2. To outline what is currently taught on planetary health in Irish medical schools;
3. To identify and address barriers and facilitators to implementing teaching on planetary health;
4. To identify key topics and learning outcomes for a planetary health curriculum;
5. To develop a proposed curriculum on planetary health for medical students.
The first workshop was held in March 2020. At this, members discussed to what extent climate and health topics are currently being integrated into the curriculum at their respective institutions. In line with the results of the PHRC, no institution in the Republic of Ireland reported comprehensive teaching on planetary health. In Northern Ireland, mapping of curriculum content to the GMC Outcomes for Graduates 2018 (General Medical Council, 2018) meant that sustainable healthcare featured as a core competence across the curriculum. Using nominal group technique, members then went on to identify key barriers and facilitators to implementing teaching on planetary health. Results are shown in Table 2.
Table 2. Key barriers and facilitators from CHIME (2021).
| Barriers | Facilitators |
| Busy curriculum | Growing importance internationally |
| Lack of staff expertise | Global mandate from SDGs |
| Uncertainty of professional relevance | Student demands |
| Culture of biomedical approach in health education | Supportive stakeholders |
| Uncertainty around what content to include | Opportunities for research |
| Funding | Interdepartmental and interdisciplinary approach |
Echoing previous studies, the main barriers discussed included an already-crowded curriculum, lack of staff expertise on the subject and an uncertainty of the relevance of the subject to clinical and academic practice. Members felt that there is a strong culture of a biomedical approach in health and healthcare education, with less focus on public health as it stands in the curriculum. Concerns were raised regarding what content to include and how this content would be weighted or examined.
With regard to facilitators, members identified a wide acknowledgement of the climate emergency internationally. It was felt that this project is a chance for Irish universities to join the ‘green wave’ and become leaders in this area. The SDGs provide a global mandate for sustainability to feature in all areas of education, and indeed, health must play a leading role in ensuring achievement of the goals by 2030. Student demands as described above provide significant leverage in making curricular change, and it was noted that the Irish Medical Council is responsive to student calls for change. Other supportive stakeholders identified included the Irish Global Health Network, the Council of Deans, the Health Service Executive, the UK-based PHEMS (Public Health Educators in Medical Schools), INHED (Irish Network of Healthcare Educators) and Coalition 2030. Fostering a relationship and discourse between academic public health departments in Ireland was recognised as a significant enabler, as was the growing importance of interdisciplinary collaboration in education.
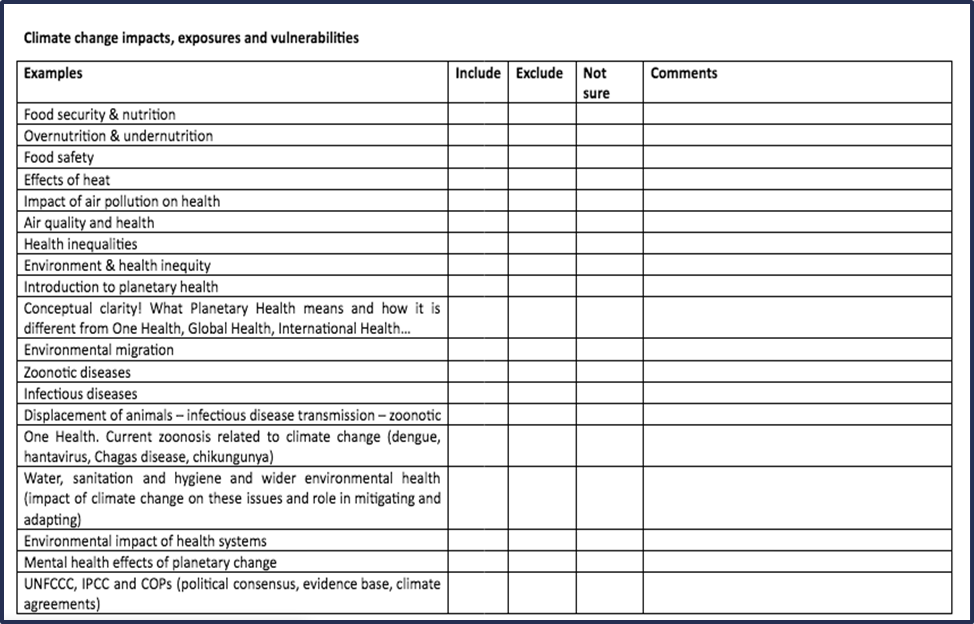
The second CHIME meeting was held in March 2021 via an online platform. At this meeting, members moved on to identifying key topics to include in a planetary health curriculum. Using Jamboard, members brainstormed various issues and areas relevant to climate, biodiversity and health. Suggestions were then reviewed and grouped under five headings taken from The Lancet Countdown Report (Watts et al., 2018) to provide an initial framework:
1. Climate change impacts, exposures and vulnerabilities;
2. Mitigation actions and health co-benefits;
3. Adaptation, planning and resilience for health;
4. Public and political engagement;
5. Implications for practice.
This proposed framework was circulated to members after the workshop, and members were invited to vote and comment on whether to include or exclude specific topics. From this, the key curriculum topics were identified (see Figure 2).
Figure 2. ‘Example of the initial framework’ (CHIME, 2021).
The overriding aim of this curriculum is to develop an ‘eco-medical’ literacy amongst undergraduates: ‘The ability to access, understand, integrate and use information about the health-related ecological effects of climate change to deliver and improve medical services’ (Bell, 2010: 3).
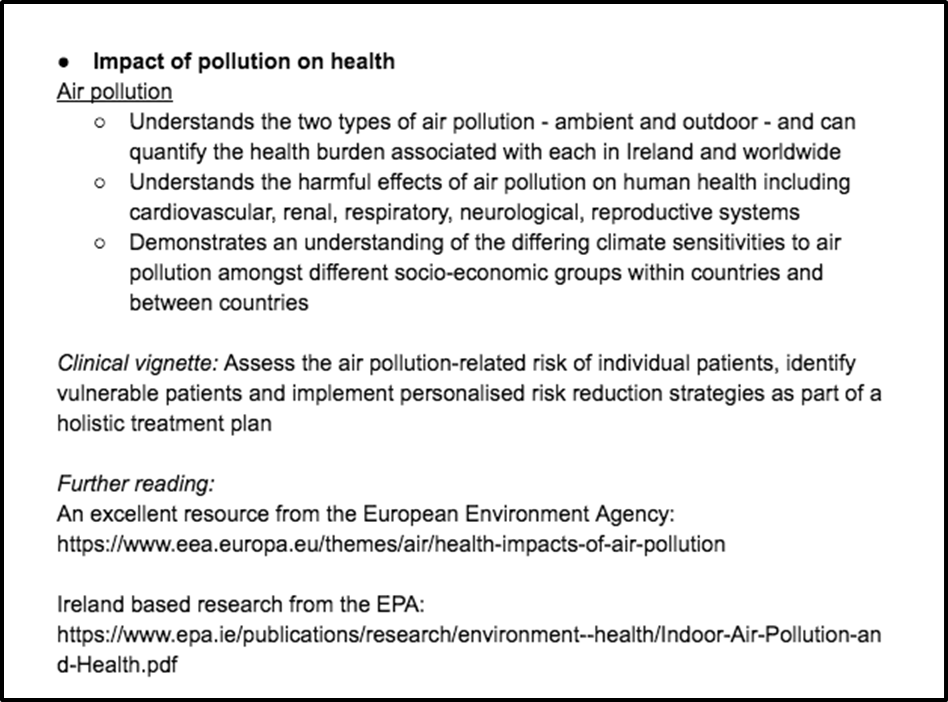
The curriculum aims to equip students with the knowledge and tools to recognise changing clinical presentations and to work in the changing clinical setting that will arise as a result of climate change and biodiversity loss. It will instil a sense within students of the link between planetary health and human rights, in particular the importance of climate justice: intersectional, intergenerational and international equity. It also aims to help students become advocates for meaningful and rapid climate action in their communities and society at large, in order to minimise the health effects of climate change and help their profession and their patients adapt to a rapidly warming world. Two to three learning outcomes were developed for each key topic, along with a clinical vignette to demonstrate relevance to clinical practice, addressing that as a barrier. Additional reading was also suggested. The example of air pollution is provided in Figure 3.
Figure 3. Example of a key topic and learning outcomes (CHIME, 2021).
In November 2021, the work of CHIME was presented at the European Public Health 2021 Conference at a workshop on planetary health curricula. Presenters from Ireland, the UK and the Netherlands discussed the work being done in their institutions and the barriers and facilitators encountered. An overarching theme was the importance of meeting universities where they already are striving to incorporate sustainability into the existing curriculum, in order to overcome the barrier of the perceived burden of adding extra content. Another benefit to this approach is that it places planetary health central to all areas of medicine, instead of being viewed as a stand-alone topic. The role of students as drivers of change and the need to include their voices at all stages of the process was emphasised. Students may be utilised as leaders and peer educators, removing the barrier of a lack of staff expertise.
The proposed curriculum was finalised and circulated for review to CHIME members and to medical students working with IDE. CHIME met again in February 2022 to discuss the proposed curriculum, assign learning hours and discuss assessment options. Three models of curriculum are envisioned: a basic curriculum, with the minimum essential learning content included; a middle-tier curriculum, including more detailed and expanded student activities; and the full curriculum, including all learning goals, clinical vignettes and assessment. It is hoped that in time, the curriculum will later be taken up at a more senior level in the medical schools for consideration, and implemented more widely across the curriculum. In doing this, CHIME aims to overcome the barrier of uncertainty around content for a planetary health curriculum and facilitate universities to incorporate content based on their capacity.
Where do we go from here?
Through our collaborative work, CHIME has provided medical schools in Ireland with the tools to overcome many of the barriers to implementing teaching on planetary health. Along with IDE and the student representatives, we envision the implementation of a planetary health curriculum into all medical schools in Ireland over the coming years. Irish medical schools have a unique opportunity to achieve the first nationwide implementation of medical teaching in this area. It is hoped that the medical schools will take advantage of this opportunity to increase the content and quality of their planetary health education and that CHIME can provide a forum for sharing of ideas and experiences between schools. In addition, the work of CHIME may serve as an example to educators from other health professions. The learning outcomes developed could be used or adapted by other health courses, thus expanding planetary health teaching to a wider field of health professionals, all of whom will have their role to play in the response to the climate crisis.
In terms of broader support across Europe, the Association of Medical Education in Europe (AMEE) released a Consensus Statement on planetary health in 2021 (Shaw et al., 2021). In this, the authors reference a study by Otto et al. (2020) which recognises that education has an essential role in attaining the SDGs and stabilising the earth’s climate by 2050. Thus, Shaw et al. (2021: 275) conclude, ‘we must rapidly mobilise health professions educators to deliver education for sustainable healthcare’. The CHIME network continues to co-operate with educators across Europe working on similar projects, fostering links for shared research and development. A changing climate requires a changing curriculum, and educators must build on the global momentum with the urgency that this crisis deserves.
There is a common purpose to the work of CHIME and that of development education in seeking the integration of international development issues into formal education. It is impossible to teach or study planetary health without referencing international development issues such as colonialism, indigenous rights, gender balance and intergenerational equity. In the setting of the current climate crisis and its link to human rights, it is negligent for medical schools to produce graduates that are not well-versed in international development and health concerns. There is a potential opportunity here for the Irish Development Education Association (IDEA) to expand their work into the field of medical education by collaborating with CHIME on developing this content. IDEA may be well-placed to provide expertise on an area not typically associated with or studied by healthcare educators. Such a partnership may allow IDEA to expand and diversify its membership by finding members from the medical field.
References
Atwoli, L, Baqui, A, Benfield, T, Bosurgi, R, Godlee, F and Hancocks, S et al. (2021) ‘Call for emergency action to limit global temperature increases, restore biodiversity, and protect health’, BMJ, No. 1734, pp. 1-3.
Bell, E J (2010) ‘Climate change: what competencies and which medical education and training approaches?’, BMC Medical Education, Vol. 10 10 (1), No. 31, pp. 1-8.
Carbon Brief (2022) available: https://www.carbonbrief.org/healthcare-in-worlds-largest-economies-accounts-for-4-of-global-emissions (accessed 14 February 2022).
CFMS (2019) ‘CFMS Health and Environment Adaptive Responsive Task Force (HEART) Planetary Health Educational Competencies’, Canadian Federation of Medical Students, available: https://www.cfms.org/files/HEART/HEART%20Competencies%20-%20Updated%20Sep%202019%20(1).pdf (accessed 14 February 2022).
CHIME (2021) available: https://www.rcsi.com/dublin/about/faculty-of-medicine-and-health-sciences/academic-departments/public-health-and-epidemiology (accessed 18 February 2022).
Climate Action Tracker (2021) ‘Glasgow’s 2030 credibility gap: net zero’s lip service to climate action’, available: https://climateactiontracker.org/publications/glasgows-2030-credibility-gap-net-zeros-lip-service-to-climate-action/ (accessed 14 February 2022).
Collins, E, Ross, J, Crawley, J and Thompson, R (2018) ‘An undergraduate educational model for developing sustainable nursing practice: A New Zealand perspective’, Nurse Education Today, Vol. 61, pp. 264-268.
CSH (Centre for Sustainable Healthcare) (2022) available: https://sustainablehealthcare.org.uk/ (accessed 18 February 2022).
Finkel, M (2019) ‘A call for action: integrating climate change into the medical school curriculum’, Perspectives On Medical Education, Vol. 8, No. 12, pp. 265-266.
General Medical Council (2018) ‘Outcome for Graduates 2018’, General Medical Council,. available: https://www.gmc-uk.org/-/media/documents/dc11326-outcomes-for-graduates-2018_pdf-75040796.pdf (accessed 2 February 2022).
Gómez, A, Balsari, S, Nusbaum, J, Heerboth, A and Lemery, J (2013) ‘Perspective: Environment, Biodiveristy and the Education of the Physician of the Future’, Academic Medicine, Vol. 8, No. 22, pp. 168-172.
Green, M and Legard, C (2020) ‘Peer-teaching could help bring sustainable healthcare into the medical education curriculum’, Med Teach, Vol. 42, No. 5, pp. 598-599.
Hackett, F, Got, T, Kitching, G T, MacQueen, K and Cohen, A (2020) ‘Training Canadian doctors for the health challenges of climate change’, Lancet Planet Health, Vol. 4, No. 1, pp. e2-e3.
Haines, A and Patz, J A (2004) ‘Health effects of climate change’, JAMA, 7 January, Vol. 291No. 1, pp. 99-103.
Hampshire, K, Ndovu, A, Bhambhvani, H and Iverson, N (2021) ‘Perspectives on climate change in medical school curricula - A survey of U.S. medical students’, The Journal Of Climate Change and Health, Vol. 4, 100033.
Huss, N, Ikiugu, M N, Hackett, F, Sheffield, P E, Palipane, N and Groome, J (2020) ‘Education for sustainable health care: From learning to professional practice’, Med Teach, Vol. 42, No. 10, pp. 1097-1101.
IFMSA (2018) ‘Statement of the International Federation of Medical Students’ Associations Sixty-fifth Session of the WHO Regional Committee for the Eastern Mediterranean Agenda Item 5 (c)’, Draft WHO global strategy on health, environment and climate change, available: https://ifmsa.org/wp-content/uploads/2018/10/IFMSA-Statement-5c_health_environment_climate_change.pdf (accessed 02 February 2022).
IPBES (2019) ‘Global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services’ in E S Brondizio, J Settele, S Díaz and H T Ngo (eds.) IPBES secretariat, Bonn, Germany.
IPCC (2018) ‘Summary for Policymakers’ in Global Warming of 1.5°C. An IPCC Special Report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty [Masson-Delmotte, V, P Zhai, H-O Pörtner, D Roberts, J Skea, P R Shukla, A Pirani, W Moufouma-Okia, C Péan, R Pidcock, S Connors, J B R Matthews, Y Chen, X Zhou, M I Gomis, E Lonnoy, T Maycock, M Tignor, and T Waterfield (eds.)]. World Meteorological Organization: Geneva, Switzerland, p. 32.
IPCC (2021) ‘Climate Change 2021: The Physical Science Basis. Contribution of Working Group I to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change’ Summary for Policy Makers, [Masson-Delmotte, V, P Zhai, A Pirani, S L Connors, C Péan, S Berger, N Caud, Y Chen, L Goldfarb, M I Gomis, M Huang, K Leitzell, E Lonnoy, J B R Matthews, T K Maycock, T Waterfield, O Yelekçi,, R Yu, and B Zhou (eds.)] Cambridge University Press. In Press.
Iroku-Malize, T, Keber, B and Philippe, N (2017) ‘Implementing Planetary Health Competencies into Medical Education’, Annals of Global Health, Vol. 83, No. 1, pp. 91-92.
Liao, W, Yang, L, Zhong, S, Hess, J, Wang, Q, Bao, J and Huang, C (2019) ‘Preparing the next generation of health professionals to tackle climate change: Are China's medical students ready?’, Environmental Research, Vol. 168 pp. 270-277.
Maxwell, J and Blashki, G (2016) ‘Teaching About Climate Change in Medical Education: An Opportunity’, J Public Health Res, Vol. 5, No. 1, p. 673.
McKimm, J and McLean, M (2011) ‘Developing a global health practitioner: time to act?’ Med Teach, Vol. 33, No. 8, pp. 626-631.
McLean, M, Gibbs, T and McKimm, J (2020) ‘Educating for planetary health and environmentally sustainable health care: Responding with urgency’, Med Teach, Vol. 42, No. 10, pp. 1082-1084.
Musaeus, P, Wellbery, C, Walpole, S, Rother, H A, Vyas, A and Leedham-Green, K (2018) ‘E-collaborating for environmentally sustainable health curricula’, Climate Change Management, Climate Change Management: Springer, pp. 151-167.
Myers, S (2017) ‘Planetary health: protecting human health on a rapidly changing planet’, The Lancet, Vol. 390, No. 10114, pp. 2860-2868.
National Health Service (2020) ‘Delivering a Net Zero National Health Service’, available: delivering-a-net-zero-national-health-service.pdf (england.nhs.uk) (accessed 14 February 2022).
NurSuS (2022) available: http://nursus.eu/uk/ (accessed 17 February 2022).
Omrani, O, Dafallah, A, Paniello Castillo, B, Amaro, B, Taneja, S and Amzil, M et al. (2020) ‘Envisioning planetary health in every medical curriculum: An international medical student organization’s perspective’, Medical Teacher, Vol. 42, No. 10, pp. 1107-1111.
Otto, I, Donges, J, Cremades, R, Bhowmik, A, Hewitt, R and Lucht, W et al. (2020) ‘Social tipping dynamics for stabilizing Earth’s climate by 2050’, Proceedings Of The National Academy Of Sciences, Vol. 117, No. 5, pp. 2354-2365.
PHA (Planetary Health Alliance) (2022) ‘Planetary Health’, available: https://www.planetaryhealthalliance.org/planetary-health (accessed 18 February 2022).
PHRC (2021) ‘Planetary Health Report Card: 2020-2021 Summary Report’, Planetary Health Report Card Initiative, available: https://phreportcard.org/wp-content/uploads/2021/04/2021-phrc-summary-report-final-1.pdf (accessed 18 February 2022).
Rabin, B M, Laney, E B and Philipsborn, R P (2020) ‘The Unique Role of Medical Students in Catalyzing Climate Change Education’, Journal of Medical Education and Curricular Development, 7.
Romanello, M, McGushin, A, Di Napoli, C, Drummond, P, Hughes, N and Jamart, L et al. (2021) ‘The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future’, The Lancet, Vol. 398, No. 10311, pp. 1619-1662.
Ryan, E C, Dubrow, R and Sherman, J D (2020) ‘Medical, nursing, and physician assistant student knowledge and attitudes toward climate change, pollution, and resource conservation in health care’, BMC Medical Education, Vol. 20, No. 1, p. 200.
Shah, S and Owusu-Addo, A (2021) ‘Envisioning planetary health in every medical curriculum: A medical student’s perspective’, Medical Teacher, pp. 484–485.
Shaw, E, Walpole, S, McLean, M, Alvarez-Nieto, C, Barna, S and Bazin, K et al (2021) ‘AMEE Consensus Statement: Planetary health and education for sustainable healthcare’, Medical Teacher, Vol. 43, No. 3, pp. 272-286.
Teherani, A, Nishimura, H, Apatira, L, Newman, T and Ryan, S (2017) ‘Identification of core objectives for teaching sustainable healthcare education’, Med Educ Online, Vol. 22, No. 11, 1386042.
Thompson, T, Walpole, S, Braithwaite, I, Inman, A, Barna, S and Mortimer, F (2014) ‘Learning objectives for sustainable health care’, The Lancet, Vol. 384, No. 9958, pp. 1924-1925.
Tun, S (2019) ‘Fulfilling a new obligation: Teaching and learning of sustainable healthcare in the medical education curriculum’, Medical Teacher, Vol. 41, No. 10, pp. 1168-1177.
United Nations (2022a) Population, New York: United Nations, available: https://www.un.org/en/global-issues/population (accessed 14 February 2022).
United Nations (2022b) ‘Secretary-General Calls Latest IPCC Climate Report “Code Red for Humanity”, Stressing “Irrefutable” Evidence of Human Influence’, 9 August, Press Release, available: https://www.un.org/press/en/2021/sgsm20847.doc.htm. (accessed 15 February 2022).
UN Department of Economic and Social Affairs (2022) ‘The 17 Goals’, available: https://sdgs.un.org/goals (accessed 18 February 2022).
United Nations Population Fund (2022) World Population Dashboard, available: https://www.unfpa.org/data/world-population-dashboard (accessed 14 February 2022).
Vlachogianni, T and Valavanidis, A (2013) ‘Energy and Environmental Impact on the Biosphere Energy Flow, Storage and Conversion in Human Civilization’, American Journal Of Educational Research, Vol. 1, No. 3, pp. 68-78.
Walpole, S C, Mortimer, F, Inman, A, Braithwaite, I and Thompson, T (2015) ‘Exploring emerging learning needs: a UK-wide consultation on environmental sustainability learning objectives for medical education’, International Journal of Medical Education, Vol. 6, pp. 191–200.
Walpole, S C, Pearson, D, Coad, J and Barna, S (2016) ‘What do tomorrow's doctors need to learn about ecosystems? - A BEME Systematic Review’, BEME Guide No. 36, Med Teach, Vol. 38, No. 4, pp. 338-352.
Walpole, S and Mortimer, F (2017) ‘Evaluation of a collaborative project to develop sustainable healthcare education in eight UK medical schools’, Public Health, Vol. 150, pp. 134-148.
Walpole, S C, Barna, S, Richardson, J and Rother, H A (2019) ‘Sustainable healthcare education: integrating planetary health into clinical education’, Lancet Planet Health, Vol. 3, No. 1, pp. e6-e7.
Watts, N, Amann, M, Ayeb-Karlsson, S, Belesova, K, Bouley, T and Boykoff, M et al. (2018) ‘The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health’, The Lancet, Vol. 391, No. 10120, pp. 581-630.
Whitmee, S, Haines, A, Beyrer, C, Boltz, F, Capon, A and de Souza Dias, B et al. (2015) ‘Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation–Lancet Commission on planetary health’, The Lancet, Vol. 386, No. 10007, pp. 1973-2028.
World Health Organisation (2022) ‘Climate change and health’, available: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health (accessed 15 February 2022).
Disclosure of Interests: Dr. Sadhbh Lee, Ms. Esmeralda Cecilie Perez, Dr. Oisin Brady Bates and Dr. Callum Swift are members of Irish Doctors for the Environment (IDE). Irish Doctors for the Environment is a registered charity consisting of doctors, medical students and allied healthcare professionals in Ireland who aim to create awareness and implement action around environmental health and the impact it has on our patients’ health. IDE receives no external funding. No funding was received for this article.
Sadhbh Lee is a doctor specialising in obstetrics and gynaecology. She is an honorary clinical lecturer at the Royal College of Surgeons Ireland. She is a founding member of Irish Doctors for the Environment, and chairs their working group on developing a planetary health curriculum. Alongside Dr. Debbi Stanistreet, she leads Climate and Health in Medical Education (CHIME) Ireland. She is a board member of the Irish Global Health Network and a former graduate of the International Academy’s Young Physician Leader programme. Email: lees5@tcd.ie.
Oisin Brady Bates is a medical doctor currently on the Trinity College Dublin general practice specialist training scheme. He is the lead of the Vasco De Gama Network's planetary health special interest group. He is a trainee representative on the Irish College of General Practitioners global health special interest group and a member of Irish Doctors for the Environment. He has a special interest in medical education. To this end he was recently awarded an MSc by research at the Royal College of Surgeons in Ireland that explored the barriers and facilitators to the integration of planetary health topics in undergraduate medical curriculum.
Esmeralda Cecilie Perez is a third-year medical student at National University of Ireland, Galway (NUIG). She is the student lead for the medical curriculum working group in Irish Doctors for the Environment, leading the student call for increased planetary health education in Ireland. She is also part of the medical curriculum review steering group at NUIG, and has presented on the role of medical students in advocating for planetary health curriculum change at international conferences.
Callum Swift is an Emergency Medicine Specialist Registrar based in Dublin, with a special interest in Planetary Health. He has given talks on Planetary health at national conferences and published research in the field in major international journals including the British Medical Journal. He is on the committee of Irish Doctors for the Environment and, as part of their curriculum working group, is helping to develop an all-Ireland Planetary health medicals school curriculum.
Debbi Stanistreet is a senior lecturer and interim Head of Department of Public Health and Epidemiology at the Royal College of Surgeons Ireland. She is the lead for CHIME Ireland alongside Dr. Lee. Originally qualifying as a nurse, Debbi later attended university as a mature student and gained a BA (Hons) in Health Studies and a Master of Public Health (MPH) before embarking on a part-time mixed methods PhD in the Department of Public Health at the University of Liverpool (UoL). She completed her PhD in 2001. Debbi worked as a lecturer / senior lecturer in public health at the University of Liverpool from 1996 to 2018, developing and teaching post graduate public health programmes both online and on campus including an online global MPH programme. She is an active researcher in the field of Household Air Pollution and continues to collaborate with the University of Liverpool ‘Energy, Air Pollution and Health’ Research Group.





